Vascular Disease – Introduction
In 2011 cardiovascular disease, that is illness due to the blockage of arteries (blood vessels that take blood from the heart to the body), accounted for 15% of all illness (16% in men and 13% in women) and about 80% of this is due to premature death. Coronary artery disease (heart attacks) and strokes are the two most important contributors.
This is much better than the situation 30 years ago. In the period from 1985 to 2015, better treatments and improved health choices have led to a 70% decrease in death from cardiovascvular disease. A wonderful outcome. (CVD death rates declined by around 70%—falling from 612 to 176 per 100,000 population for males and 410 to 129 per 100,000 for females (Figure 2).
However, with 29% of all deaths in 2015 in both men and women being due to cardiovascular disease, there is still much work to do; especially with regard to reducing the incoidence of cardiovascular disease risk factors. (See table below.)
While men suffer from more cardiovasculsar disease, mainly due to it occurring at an earlier age, in 2018 about 4.8% of women over 18 years of age (510,000) had cardiovascular disease; mainly coronary heart disease (heart attacks and angina) - 40%, strokes - 35%, and heart failure - 6%.
Coronary artery disease is the disease that is most likely to cause both men and women to die prematurely, and even in people with no (known) risk factors for vascular disease, it is still the most likely cause of death. Thus, this section needs to be read by every adult; especially as many Australia adulats have multiple known risk factors. (Assessing your risk of cardiovascukar disease is discussed in detail in the Heart Attack: Assessing your risk section.
Incidence of some modifiable cardiovascular disease risk factors in adult Australians (2017) |
||
Risk Factor for vascular disease |
Incidence in adults |
|
Males |
Females |
|
Diabetes and impaired glucose tolerance |
11% (7% + 4%) |
7% (5% + 2%) |
High blood lipids (uncontrolled) |
63% (57%) |
63% (57%) |
Inadequate physical activity |
34% |
59% |
Smoking |
15% |
11% |
High blood pressure (Poorly controlled) |
34% (24%) |
34% (22%) |
Overweight (BMI > 25) |
71% |
56% |
Excessive alcohol consumption |
26% |
9.3% |
Inadequate consumption of fruit & vegetables |
Up to 90% |
Up to 90% |
An outline of the vascular (blood vessel) system
The vascular system is basically a system of tubes, known as blood vessels,used for transporting blood. Those tubes taking blood from the heart to the various organs of the body, such as the muscles, the brian and the heart muscle itself, are called arteries. Those returning blood from these organs to the heart are called veins. The power to move blood through these vessels is supplied by the heart, which is really just a pump.
The blood in the arteries takes essential nutrients, including oxygen needed for the production of energy in the body’s cells, to the body’s organs. Without an adequate supply of oxygen, cells soon die. The time it takes cells deprived of oxygen to die varies. Brain cells can last for only a few minutes. Heart muscle cells can last for up to five hours or more.
Vascular disease
It is the arteries, the vessels taking blood from the heart to the body, that are involved in vascular disease. Vascular disease acts to block these arterial vessels and, in doing this, blocks the supply of oxygen and nutrients to the tissue the artery supplies. These blockages occur in the inner section of the artery wall, adjacent to the lumen, and they occur as multiple discrete small lesions rather than as a generalised blockage along the whole length of the artery. They occur in all the arteries of most people in Western society as they age but cause the most problems in the following situations.
- Blockages in arteries supplying the heart muscle (the coronary arteries), which causes heart pain (angina) and heart attacks.
- Blockages in arteries supplying the brain (the carotid and vertebral arteries), which causing strokes.
- Blockages in arteries supplying the lower legs,which causes peripheral vascular disease. (In serious cases this results in gangrene and the need to amputate lower parts of the leg.)
- Blockages in the main artery leaving the heart, which is called the aorta. (This weakens the artery causing an aortic aneurysm that can eventually rupture causing sudden catastrophic bleeding and often death.)
- Blockages in arteries supplying the kidneys.
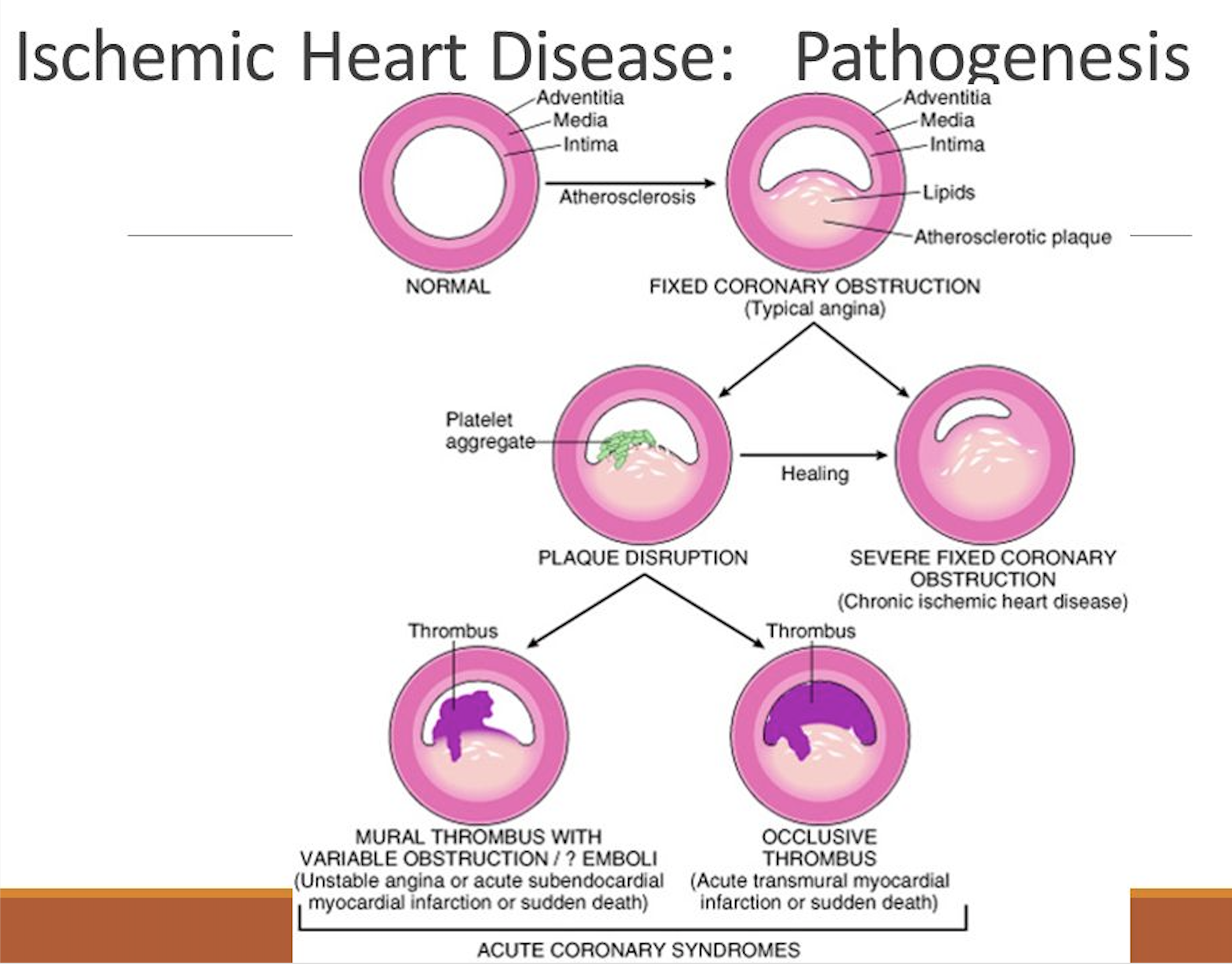
Each individual lesion is caused by a thickening of the vessel wall that occurs when cholesterol accumulates in the wall of the artery, forming a fatty lump that gradually increases in size with age. As this occurs, the tissue between the lump and the lumen of the vessel becomes progressively thinner and eventually breaks down exposing the underlying lesion. The pressure the deposition of fat causes determines how ths breakdown occurs.
1. Rupture of the lesion: If the fatty deposit causes significant pressure within the lesion, the lesion can suddenly rupture and cause a large breakdown in the internal surface lining of vessel. This is the case in about 50% of heart attack cases and is more commonly the cause of serious heart attacks.
2. Errosion of the lesion: If the fatty deposit causes little pressure within the lesion, then the breakdown often occurs more gradually as a smaller errosion of the surface. This occurs in about 50% of caes and generally causes fewer symptoms and smaller heart attacks. (Some people who have heart attacks, especially older women, can have no symptoms at all when it occurs.)
Unfortunately there are no tests available to tell which lesions are likely to break down and whether the breakdown is likely to occur as a rupture or an errosion. The development of these lesions is outlined in the following series of diagrams. Before reading this material, it is important to review the information on cholesterol in the nutrition section of this web site, especially that relating to lipoproteins. (Lipoproteins transport cholesterol in the blood.)
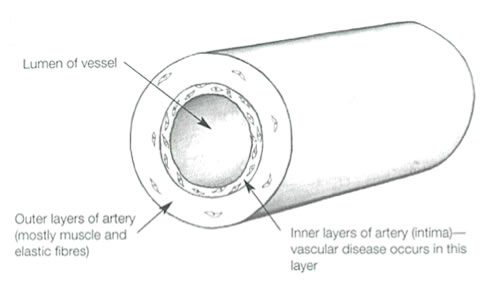
1. Normal artery (at birth)
This is a simplified view of a normal artery wall with no vascular disease present. The inner layer (or intima) is where vascular disease occurs. In Western society, vascular disease gradually increases from early in life. Even at the age of 10, many children would have signs of the early stages of vascular disease. |
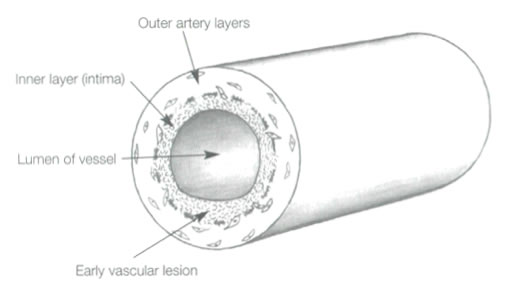
2. Early vascular disease (called a ‘fatty streak’)
A small deposit of cholesterol containing cells (‘foam cells’) and cholesterol itself has formed in the inner (‘intima’) section of the artery. These lesions often start because the inner part of the artery wall at this location was injured in some way. There are numerous possible causes for this injury, including forces associated with high blood pressure, chemical injury from compounds originating outside the body, such as chemicals from cigarette smoke, raised blood levels of normal body compounds (such as homocysteine), and perhaps even infection. Turbulent blood flow around areas where blood vessels branch is a factor that causes lesions to commonly occur in these regions.
What causes excess cholesterol to accumulate in an artery wall? Cholesterol is necessary for cells to live and its entry into cells is usually tightly controlled. Injury to the cells lining the inner artery wall makes them more prone to interact with and take up LDL cholesterol (bad cholesterol) in the blood. Other factors that increase LDL cholesterol uptake into the developing lesion include:
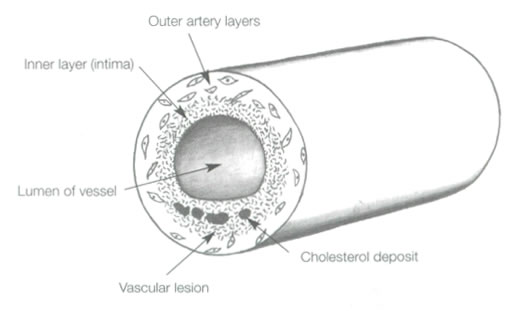
The ‘cholesterol deposit’ lesion shown above has caused a slight thickening of the intima layer of the artery and consequently reduced the size of the lumen. (This has resulted in a slight reduction in blood flow through the artery.) |
3. Further progression of vascular disease (Occurs from the third decade of life onwards)
Further enlargement of the lesion has occurred and distinct cholesterol deposits have developed. As well as containing cholesterol, the lesion has started to accumulate some fibrous connective tissue and calcium, a process that hardens the lesion.
The rate of this enlargement process depends on the number of risk factors for vascular disease the person processes and their severity. Important risk factors include:
Vascular lesions usually take about 10 to 20 years to reach this stage and such lesions are relatively common in adults in their fifties and sixties. They occur even earlier in people with a high overall risk of vascular disease.
Early lesions often expand outwatrds and thus don't cause much blockage: In the early to middle stages of lesion formation, thinkening of the artery wall often results in the artery wall expanding outwards rather than inwards. (Not shown in the above diagram.) This means that, although a lesion is present, it tends to cause less blockage. Angiograms done to determine the extent of lesions often therefore underestimate the severity of the underlying lesion because what they see is the blockage. Lesions that go on to cause heart attacks are thus not always the ones causing significant blockages. |
Possible outcomes of vascular atherosclerosis lesions
The fate of a person’s vascular lesions (and the person!) depends on how well vascular disease risk factors are looked after. People with fewer, less severe risk factors will usually develop far fewer lesions and they are more likely to appear significantly later in life. If a person has numerous risk factors, he or she can expect trouble a lot earlier.
A. Lesions can decrease in size when a person takes care of their risk factors for vascular disease
HDL cholesterol (good cholesterol) actually removes cholesterol from these lesions and improving your blood cholesterol by increasing the HDL (good) cholesterol level and decreasing the LDL (bad) cholesterol level can reduce leson size in this way. This can be achieved through consuming a diet with a healthy fat intake or by taking cholesterol lowering medication.
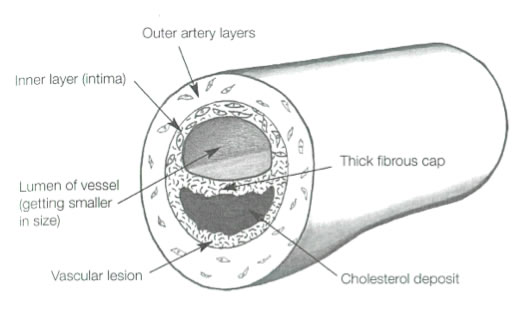
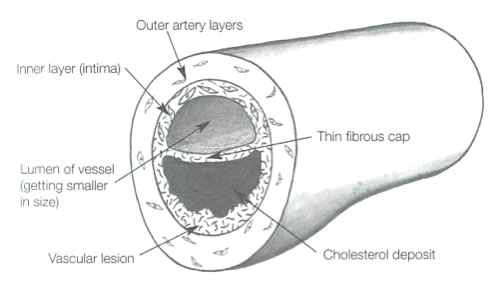
B. Lesions can increase in size – Stable and unstable lesions
In people with significant vascular disease risk factors, the lesions are likely to get larger. With further lesion enlargement, the blood vessel (artery) becomes more blocked and a distinct layer (a fibrous cap) develops between the lesion and the artery lumen. This cap can be either thick (Diagram 4) or thin (Diagram 5) and this greatly affects the subsequent development of the lesion.
4. Established lesion with a thick capsule – A stable lesion (Generally occurs after the age of fifty and is most common in people aged over seventy years.)
If the inner wall cap is thick, the lesion usually just continues to gradually increase in size, resulting in a corresponding decrease in the size of the vessel lumen. These are called stable lesions.
The body can compensate, to a degree, for the gradual decrease in the lumen size of a vessel by making new smaller vessels to bypass the increasingly blocked vessel (artery). However, the blockage will eventually become large enough to cause problems due to inadequate supply of blood (and thus inadequate supply of oxygen) to the tissue the artery supplies. Initially this causes symptoms only when the person is exercising, as muscle tissue requires more oxygen during exercise. However, the blockage may eventually become large enough to cause symptoms even when the person is resting. (An example of this process is chest / heart pain (angina), which occurs when heart muscle tissue does not receive enough oxygen. Angina pain is more likely to occur during exercise.)
These types of lesions are more common in people with more favourable vascular disease risk factors and these people are also more likely to develop such lesions later in life. |

A cross section through a real coronary artery with significant vascular disease (atherosclerosos) similar to diagram 4.
5. Established lesion with a thin capsule – An unstable lesion (Generally occurs after the age of fifty and is most common in people aged over seventy years.)
If the vascular lesion is covered by a thin and thus weaker fibrous cap, it is more likely to tear or rupture. These are called unstable lesions. Thin fibrous caps form over lesions for several reasons, including increasing pressure on the fibrous cap from a relatively rapidly enlarging underlying cholesterol deposit and further injury (and inflammation) to the inner lining of the vessel or the cap itself. Lesions with thin caps are more likely to occur in people with multiple, more severe risk factors.
These lesions are far more likely to rupture. (See Diagram 6.)
Aggressively reducing risk factors can reduce the size of the cholesterol deposits in these unstable lesions, thus reducing both the pressure exerted on the thin cap and the irritation that the cholesterol deposit exerts on the cap tissue. This can reduce the likelihood of 'cap rupture'. It’s a bit like letting some air out of an overfilled balloon that is likely to rupture. |
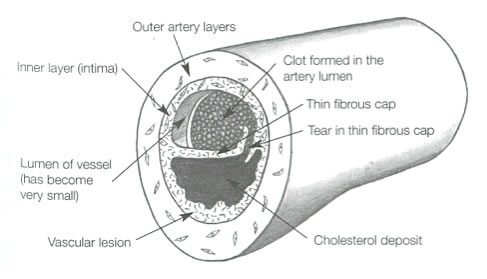
6. Lesion breakdown
a. Lesion rupture (sudden, larger and more dramatic) - 50% of cases
(Generally occurs after the age of fifty and is most common in people aged over seventy years.)
When this weakening process is severe enough, the thin cap of the unstable lesion will tear or rupture. This brings the underlying cholesterol deposit into direct contact with blood in the artery lumen. The natural response of the body is to repair this break and the body starts this process by quickly (in few minutes) establishing a blood clot over the rupture site. This clot formation is important a it often significantly increases the blockage the lesion causes.
The consequence of this rupture and clot formation depends on the degree of blockage it causes. A large blockage will cause a dramatic reduction in blood flow through the artery and an equally large reduction in the oxygen it delivers to the tissues it supplies and this usually results in the death of this tissue. This is how almost all heart attacks and many strokes occur. If the rupture is not this large, it may just cause symptoms to occur with exercise and no permanent damage. Smaller ruptures may even give no symptoms but all such ruptures act to further weaken the inner vessel wall and make future larger ruptures much more likely.
About half of all heart attacks (and the majority of severe heart attacks and deaths due to heart attacks) occur from ruptures to unstable lesions that, prior to rupturing, caused much less severe blockage; usually a blockage of less than 40% of the artery lumen. These smaller blockages are usually not able to be detected by stress tests or ECGs and give no warning symptoms before the heart attack occurs. Thus, many, many heart attacks occur 'out of the blue', with no prior warning. Prevention is the only hope!!
b. Lesion errosion (less dramatic) - also about 50% of cases
When the build up of fat in the vascular lesion causes less pressure, the breakdown process can be more gradual and less dramatic. In this case, the tissue lying between the lesion and the lumen can just errode and the area of breakdown occurs more gradually and issmaller. The clot that forms over this area is therefore also smaller and thus causes less blockage. Thus, these lesions cause smaller less significant heart attacks or just angina pain with exercise.
As stated previously, there are no tests available that can reliably tell whether an existing lesion is going to breadown and whether this breakdown will occur as a rupture or an errosion.
Removal of clots
When a heart attacks occurs, quickly removing the clot that forms over a vessel rupture (by drugs or surgery) can avoid or significantly reduce permanent damage to heart muscle. This is one reason why anyone with symptoms suggestive of a heart attack needs to go to hospital as quickly as possible (by ambulance). Every minute counts!
Aspirin: A single aspirin tablet can help this ‘clot-removing’ process and should be taken as soon as a heart attack is suspected unless the person is allergic / has serious side effects to aspirin.) Heart attack symptoms are described in the section 'Heart attacks and strokes - General information'.
Similarly, people with a suspected stroke need to be assessed in hospital quickly to minimise brain damage. |
Further information
National Heart Foundation
Their ‘Heart line’ information service Ph 1300 362 787